Bad IVF News? What to Do Next - From the Lab’s Perspective
Hearing disappointing IVF results can be devastating, but understanding the laboratory findings can help you make informed decisions about your next steps. Here's what embryologists wish patients knew when facing challenging outcomes.
Decoding Common Scenarios and Lab Insights
1. "No Embryos Made It to Blastocyst"
What the lab sees:
Arrest at cleavage stage (Days 2-3)
Failure to compact (Day 4)
Early blastocyst collapse (Day 5)
Possible causes:
Chromosomal abnormalities (60-80% of cases)
Sperm DNA fragmentation
Mitochondrial dysfunction
Suboptimal culture conditions
Lab-recommended next steps:
Request detailed embryo development notes
Consider PGT-A testing in future cycles
Discuss culture media alternatives
Evaluate sperm DNA fragmentation testing
2. "All Embryos Were Poor Quality"
Grading reality check:
CC-graded (3CC, 4CC, etc.) blastocysts have <15% implantation rate
Severe fragmentation (>25%) reduces viability
Asymmetric cell division impacts the potential
Lab perspective:
"Poor quality" often reflects chromosomal issues
Some "ugly" embryos can still be genetically normal
Morphology doesn't always predict function
Action items:
Review time-lapse videos if available
Ask about rescue ICSI for future cycles
Consider co-culture systems if repeated
3. "Fertilization Failed"
Behind the lab door:
0PN (no pronuclei) vs 1PN (one pronucleus) outcomes
Post-ICSI degeneration rates
Sperm binding/activation issues
Technical solutions:
Calcium ionophore activation (for egg activation deficiency)
PICSI sperm selection (for binding issues)
Polarized light microscopy for spindle detection
The Lab's Problem-Solving Toolkit
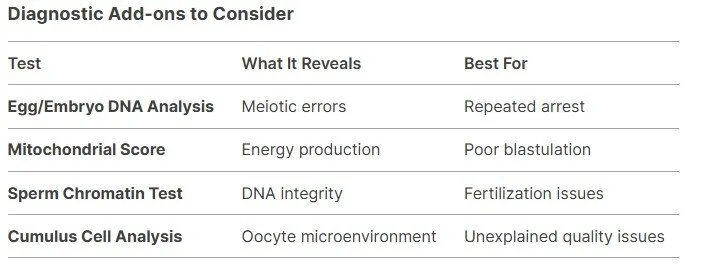
There are a few things the lab can do. We’ve included a graphic below, but keep in mind that it’s very rare for labs to perform these diagnostic measures. It’s more realistic for labs to try these assessments:
Spindle-view analysis - Checks meiotic spindle integrity for optimal ICSI timing
Check out this study by Suji Kim (2024) that found spindle-view significantly improved blastocyst transfers
Different ICSI timing - Gives eggs more time to mature for optimal ICSI timing
Physiologic ICSI (PICSI) - Captures mature sperm for ICSI
Zymot - Captures high-quality sperm for ICSI
Zona drilling - Thin the zona pellucida for less aggressive ICSI manipulation
Calcium Ionophore - Activates the egg
When to Seek a Second Opinion (From a Lab Specialist)
Red flags worth investigating:
50% embryo arrest rate in multiple cycles
Fertilization rates <30% with ICSI
Discrepancies between egg maturity and blastocyst rates
Unusually high degeneration post-thaw
What to request:
Complete embryo development records
Culture media lot numbers
Did you hear about CooperSurgical’s lawsuit regarding their culture media?
Read this story on Margarita Komarova and Colin McDarmont’s IVF tragedy
Incubator calibration reports
Embryologist certification details
The Silver Linings Labs Observe
One good embryo is enough - Many success stories start with a single fair-quality blastocyst
The IVF Kitchen believes in positivity, yet we understand how this process can wear down positivity throughout the IVF cycle. This phrase, “one good embryo is enough,” is quite common, and while it is true, many patients have had issues with the phrase. Understandably, if we all played the statistics game, then yes, more is better, but this simply isn’t the reality for most patients. For the amount of negative experiences with only having one good embryo, there is easily more positive experiences from patients who only had one good embryo, so stay strong and stay positive!
Arrest reveals problems early - Better than repeated implantation failure
Each cycle provides data - Even "failed" cycles guide better protocols
Technology keeps advancing - Today's limitations may be solved tomorrow
Your 7-Point Action Plan
Schedule a lab consult - Not just with your doctor, but with the lead embryologist
Request raw data - Developmental timelines, photos, grading sheets
Compare to lab averages - Ask how your results stack up to their typical outcomes
Review media/incubators - Some patients respond better to certain systems
Consider split trials - Test different protocols simultaneously
Explore clinical trials - Experimental approaches for tough cases
Preserve evidence - Request vitrification of arrested embryos for future analysis
Each individual's situation is unique so don’t get discouraged when reading through this perspective. Even the most difficult cases have been able to have a live birth with today’s scientific advances in the lab. Every failed IVF cycle is an opportunity to collect relevant data so that you may have a baby on the next IVF cycle. Some of our most successful patients had multiple poor cycles before we cracked their unique biological code. The IVF journey is not an easy one, but definitely the most rewarding one!
“All my brothers and sisters quit. Don’t be like them. Be like me!”