Embryo Development: What is the Ideal IVF Timeline and Checkpoints?
A question we come across often is “Is the embryo developing normally?”. This type of question can’t be answered simply, as it can be very complex and with many layers of relevant information. To be clear, embryo development should follow a specific timeline with certain key checkpoints that the lab can identify so they can deem development as good. Many companies are studying the morphokinetics of embryo development. This is analyzing embryo development by combining morphology (how the embryo looks) with kinetics (timing of key developmental events). Check out this helpful video if you’re a visual learner!
There are specific milestones assessed to optimize the chances of a successful pregnancy and understanding the ideal timeline and key checkpoints can provide valuable insights into the IVF journey.
The Standard IVF Embryo Development Timeline
Day 0: Fertilization Assessment
16-18 hours post-insemination
Key Checkpoint: Presence of two pronuclei (2PN)
What embryologists look for:
Normal fertilization (2PN)
Abnormal fertilization (0PN, 1PN, 3PN)
Polar body positioning
Success benchmark: 70-80% fertilization rate with ICSI
Day 1: Zygote Stage
24 hours post-fertilization
Expected development: Still single-cell
Quality indicators:
Clear cytoplasm
Visible pronuclear alignment
Red flags:
Multi-nucleation
Dark granular cytoplasm
Day 2: Cleavage Begins
48 hours post-fertilization
Ideal development: 2-4 cells
Grading criteria:
Cell symmetry (blastomeres of equal size)
Fragmentation percentage (<10% ideal)
Nuclear status (one nucleus per blastomere)
Arrest signs:
Failure to cleave
Severe fragmentation (>25%)
Day 3: Compaction Phase
72 hours post-fertilization
Target cell count: 6-8 cells
Critical developments:
Embryonic genome activation begins
Initial compaction starts
Morphological changes:
Cell boundaries become less distinct
Early signs of cell-to-cell adhesion
Clinical decision point:
Day 3 transfer candidates identified
Extended culture decisions made
Day 4: Morula-Cavitation Formation
96 hours post-fertilization
Key transition: Compaction completes
Hallmark features:
"Mulberry" appearance
Indistinct cell borders
Beginning of cavitation
Potential issues:
Arrested development (common checkpoint)
Partial compaction
Days 5-6: Blastocyst Stage
120-144 hours post-fertilization
Developmental milestones:
Blastocoel cavity formation
Distinct inner cell mass (ICM)
Organized trophectoderm (TE)
Grading system:
Expansion (1-6)
ICM quality (A-C)
TE quality (A-C)
Transfer window:
Most transfers occur Day 5
Some embryos need Day 6 to develop
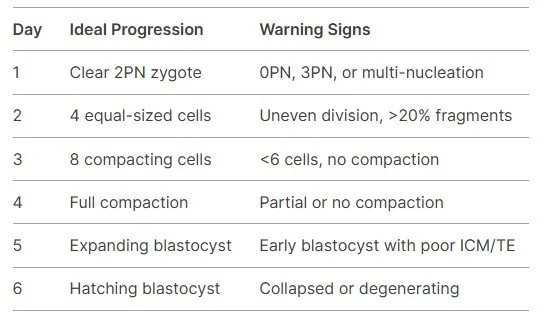
Ideal vs. Suboptimal Development Patterns
Why Timing Matters: The Biological Clock
Genome Activation:
-Maternal-to-zygotic transition occurs Day 2-3
-Late activation often indicates problems
Metabolic Shifts:
-Glycolytic activity increases at the blastocyst stage
-Abnormal metabolism may cause arrest
Cell Cycle Synchrony:
-Ideal embryos maintain precise division timing
-Asynchrony suggests chromosomal issues
Embryos that follow this timeline have a better chance of forming viable blastocysts. Key checkpoints are reached on each day and this gives the lab some idea of how well the embryo is doing.
What Happens if My Embryo Develops Slow or Fast?
Slow embryo development could be due to:
Embryo quality
Laboratory conditions
Egg or Sperm Factors
Embryo Self-Correction
Fast embryo development could be due to:
Possible chromosome abnormalities
Dr. Dieter Egli of Columbia University Vagelos College of Physicians and Surgeons found that many embryos that failed to develop have chromosomal abnormalities
Poor morphological quality
In vitro artifacts (lab conditions)
Compensatory acceleration
Regardless of whether an embryo develops slowly or fast, there is still a chance that it will become a viable blastocyst. According to Dr. Tanmoy Murkherjee, co-director of RMA of NY, implantation is still possible if you get the timing correct. This isn’t a perfect science, and it comes down to the embryo! Just like in life, some people develop faster and some develop slower, but everyone reaches the same destination.
Morphokinetics in the Lab
Companies are using AI technology with morphokinetics to predict lab outcomes. Their AI algorithm looks at embryo morphology and timeline to accurately assess whether your embryo will be genetically normal, develop to a blastocyst, implant, or even live birth! Can you imagine that?
These companies rely on time-lapse incubators and have already started being implemented in some labs. Would you pay extra for these services?
Questions to Ask Your Embryologist
✔ "What percentage of embryos typically reach the blastocyst stage in your lab?"
✔ "How do you decide between Day 3 and Day 5 transfers?"
✔ "What developmental variations would prompt concern?"
✔ "Do you provide time-lapse imaging of embryo development?"
Understanding these stages and checkpoints allows patients and clinicians to make informed decisions throughout the IVF process, aiming to enhance the likelihood of a successful outcome!
“We watch these embryos like a Netflix series—every day a new episode, every division a plot twist. Day 2? Cliffhanger. Day 5? Season finale.”