Semen Analysis Report: What Sperm Count, Motility & Morphology Mean
If you're undergoing fertility testing, one of the first steps often includes a semen analysis. This test evaluates the health and viability of a man's sperm and is essential for diagnosing male infertility. The report might look like a sheet of confusing numbers and medical terms—but each parameter tells an important story about fertility potential. Here’s a breakdown of the key components: sperm count, motility, and morphology—and what they really mean.
Sperm Count: How Many Are There?
Sperm count refers to the total number of sperm present in a semen sample. A normal count, according to the World Health Organization (WHO), is at least 15 million sperm per milliliter of semen. Anything below this is referred to as oligospermia. A complete absence of sperm is called azoospermia.
What It Measures:
Concentration: Number of sperm per milliliter (mL) of semen.
Total Count: Total sperm in the entire ejaculate (concentration × semen volume).
WHO 6th Edition Reference Values
Sperm count refers to the total number of sperm present in a semen sample. A normal count, according to the World Health Organization (WHO), is at least 15 million sperm per milliliter of semen. Anything below this is referred to as oligospermia. A complete absence of sperm is called azoospermia.
Low count (oligospermia): Can result from varicoceles, hormonal imbalances, infections, or lifestyle factors (e.g., smoking, heat exposure).
Azoospermia: No sperm in the ejaculate (requires further testing for blockages or production issues).
Low sperm count doesn’t always mean natural conception is impossible, but it can make it harder—especially if other parameters like motility or morphology are also poor. In IVF, lower counts may prompt your doctor to suggest ICSI (Intracytoplasmic Sperm Injection), where a single sperm is directly injected into the egg.
Next Steps for Low Count:
Repeat the test (sperm counts fluctuate).
Evaluate for varicoceles or hormonal issues (FSH, testosterone tests).
Consider IVF with ICSI for severe cases.
Sperm Motility: Can They Swim?
Motility measures how well sperm move, which is vital for reaching and penetrating the egg. Sperm are graded into:
Progressive motility: Sperm move in a straight, purposeful direction (most important for natural conception).
Non-progressive motility: Sperm move, but not efficiently and in a purposeful direction.
Immotile: Sperm don’t move at all.
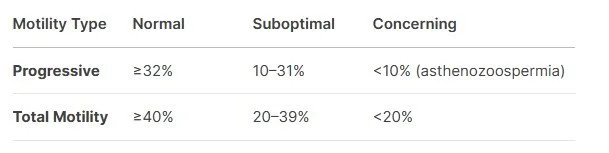
WHO Thresholds
A normal sample has at least 40% motile sperm, with 32% showing progressive movement. Poor motility, known as asthenozoospermia, can reduce the likelihood of sperm reaching the egg—even during IVF—unless ICSI is used.
Why It Matters:
Poor motility limits sperm’s ability to reach and fertilize the egg.
Even with IVF/ICSI, low motility may signal DNA damage (test for fragmentation if motility <40%).
Causes of Poor Motility:
Oxidative stress (smoking, pollution).
Varicoceles.
Infections (e.g., prostatitis).
Morphology: Are They the Right Shape?
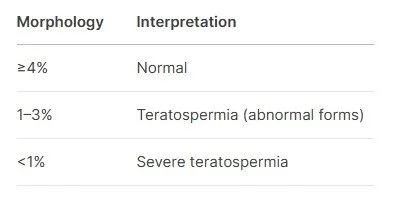
Morphology refers to the structure and shape of the sperm, including the head, midpiece, and tail. Abnormal morphology may impair a sperm’s ability to fertilize an egg. Morphology is measured using strict Kruger criteria, and 4% or more normal forms is considered acceptable by WHO standards.
What It Measures:
Kruger Strict Criteria: Evaluates head, midpiece, and tail shape.
Normal Morphology: ≥4% of sperm with ideal form.
Don’t be alarmed if your morphology seems low—this is one of the strictest fertility measures. Even men with <4% normal forms can still conceive, especially with assistance like ICSI. However, poor morphology may be associated with higher DNA fragmentation, which can affect embryo quality.
Why It Matters:
Misshapen sperm may struggle to penetrate the egg.
ICSI can bypass morphology issues, but severe abnormalities (e.g., globozoospermia) may require specialized treatment.
Causes of Poor Morphology:
Genetic factors.
Oxidative stress.
Other Important Parameters
Your semen analysis may also include:
Volume: Normally 1.5–6.8 mL per ejaculate.
pH: Should be slightly alkaline (7.2–8.0).
White blood cells: High levels may indicate infection.
Sperm vitality: Checks whether non-moving sperm are dead or alive.
Did you know men with higher-quality sperm might live longer? Check it out in this article!
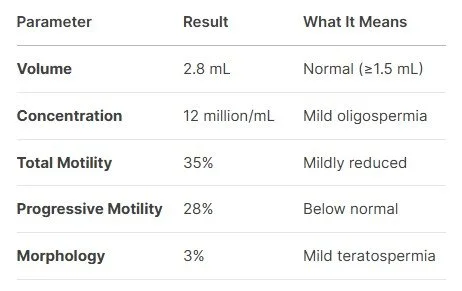
Sample Report Interpretation
Next Steps for This Report:
Repeat the test in 3 months (sperm regenerates every ~74 days).
Lifestyle changes: Quit smoking, avoid hot tubs, wear loose underwear.
Test DNA fragmentation (linked to low motility/morphology).
Consult a reproductive urologist to check for varicoceles or hormonal issues.
What If My Results Aren’t Normal?
An abnormal semen analysis doesn’t automatically mean infertility. Many issues can be treated or improved over time. Lifestyle changes, medications, or procedures like varicocele repair or sperm retrieval may be options.
Also, a single test isn't always definitive. Repeat testing is usually recommended, as sperm quality can fluctuate due to illness, stress, or lifestyle factors. If you’ve been following our stories, then you know in the last blog that we’ve had many male patients who came with poor semen samples, but were able to turn things around with changes in diet and lifestyle! There’s definitely hope because sperm is constantly being replenished.
Bottom Line
A semen analysis gives vital insight into male fertility—but interpreting the results requires context. Work with your clinical team to understand what your numbers mean and what your next steps should be. In many cases, even significantly abnormal results can still lead to a successful pregnancy with the right approach.
One abnormal test ≠ infertility: Repeat testing is crucial.
Lifestyle changes work: Quit smoking, reduce alcohol, and manage stress.
ICSI overcomes many issues: Even with low counts or poor morphology.
DNA health matters: Fragmentation testing is key if motility/morphology are low.
“I could have told you that.”