What are TESE, TESA, MicroTESE, MESA, and PESA? Sperm Extraction Methods for IVF
Azoospermia is a condition where no sperm is found in the ejaculate. This is uncommon and affects roughly 1% of all men; however, it contributes to 10-15% of all male infertility cases. Have no fear, as there are a variety of ways to deal with this. Let’s talk about sperm extraction methods for IVF!
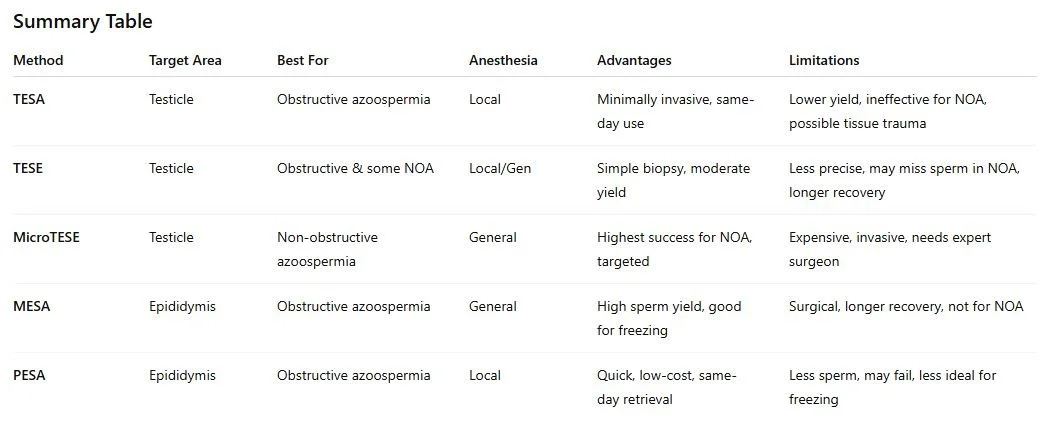
IVF with sperm extraction offers a real chance at biological fatherhood. But not all sperm retrieval methods are the same. Five major techniques: TESA, TESE, MESA, MicroTESE, and PESA, are used based on the cause of infertility (obstructive vs. non-obstructive), and each has specific protocols, risks, and success rates.
Let’s explore these sperm extraction techniques in depth.
1. TESA – Testicular Sperm Aspiration
What it is:
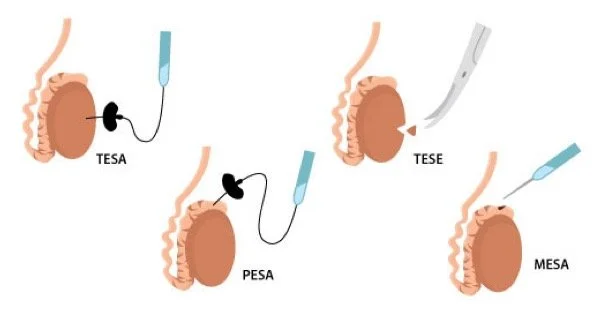
TESA is a minimally invasive procedure where a fine needle is used to aspirate sperm directly from the testicle.
When used:
Primarily for obstructive azoospermia, such as post-vasectomy or congenital vas deferens absence. Occasionally used in non-obstructive cases as a first step.
Details:
Done under local anesthesia.
Involves a small needle puncture (no incision).
Performed in-office or alongside egg retrieval.
Sperm is extracted and immediately processed for ICSI.
Limitations:
Lower sperm yield compared to surgical methods.
May not retrieve sperm in cases of non-obstructive azoospermia.
Tissue damage can occur if multiple attempts are made.
2. TESE – Testicular Sperm Extraction
What it is:
A surgical biopsy of the testicular tissue through a small incision in the scrotum. Tissue is then examined under a microscope in the lab for the presence of sperm.
When used:
It can be used for both obstructive and non-obstructive azoospermia.
Details:
Requires local or general anesthesia.
Simple incision and tissue removal.
Less targeted than MicroTESE.
Often yields enough sperm for immediate or future IVF/ICSI cycles.
Limitations:
Less targeted than MicroTESE.
Can cause pain, swelling, or hematoma.
Recovery time is longer than TESA.
May not find sperm in severe non-obstructive cases.
3. MicroTESE – Microsurgical Testicular Sperm Extraction
What it is:
The most advanced method for men with non-obstructive azoospermia. A high-powered operating microscope is used to identify the seminiferous tubules most likely to contain sperm, minimizing tissue removal and improving chances of sperm retrieval.
When used:
For severe male infertility due to poor sperm production (e.g., genetic disorders, Sertoli cell-only syndrome, maturation arrest).
Details:
Requires general anesthesia.
Only performed by experienced urologic microsurgeons.
Sperm retrieval rates: 30–60% for NOA (non-obstructive azoospermia) cases
Limitations:
Requires specialized microsurgical skill and training.
Expensive.
Invasive with longer recovery.
Performed only in select, experienced centers.
4. MESA – Microsurgical Epididymal Sperm Aspiration
What it is:
Microsurgical extraction of sperm from the epididymis (where sperm mature after leaving the testis) using an operating microscope.
When used:
Best for obstructive azoospermia (e.g., vasectomy, congenital blockage).
Details:
Performed under general anesthesia.
Yields a large quantity of mature, motile sperm.
Ideal for cryopreservation and multiple IVF cycles.
Limitations:
Requires a skilled microsurgeon and an operating room.
Invasive with a longer recovery than PESA.
Higher cost.
Not suitable for non-obstructive azoospermia.
5. PESA – Percutaneous Epididymal Sperm Aspiration
What it is:
A less invasive alternative to MESA. A fine needle is used to aspirate sperm from the epididymis without an incision.
When used:
Obstructive azoospermia when a less invasive option is preferred.
Details:
Done under local anesthesia.
Quick recovery.
Less precise than MESA and may yield fewer sperm.
Often a first-line approach; MESA may follow if PESA fails.
Limitations:
Less precise than MESA.
May require multiple attempts or fail to retrieve viable sperm.
Lower sperm yield and quality compared to MESA.
Reference - Shrikhande Clinic
Final Thoughts
Choosing the right sperm retrieval method depends on the cause of azoospermia and whether future IVF cycles are anticipated. Patients will need to work with a reproductive urologist and fertility clinic to discover the best extraction method possible.
The IVF Kitchen has extensive experience with these procedures and know that even the best surgeon will fail if the IVF lab team does not have the experience to retrieve the sperm after extraction surgery. Make sure your IVF clinic’s lab team has the skill and experience before scheduling sperm extraction with them!
“No sperm? No problem! Science has backup plans—and trust me, we’re resourceful little guys.”