Behind Le Microscope: A Morning in the Life of an Embryologist
When it comes to IVF, many patients focus on the procedures and the miracle of embryo transfer. However, behind every successful procedure lies the diligent work of the embryologist—often working quietly behind the scenes to create a stable, controlled environment for fertility success. As with any field where precision is paramount, the embryologist's morning routine is a key part of ensuring that everything goes according to plan.
From calibrating equipment to preparing culture media, the first hour of an embryologist’s day is packed with critical tasks that set the tone for the rest of the IVF journey. Let’s go behind the microscope and explore the meticulous morning routine that sets the stage for a successful IVF process, from the time an embryologist steps into the lab to the moment they begin working with patients' samples.
1. Entering the Lab: A Quiet Start with Intense Focus
Le calm before the storm
An embryologist's day typically starts early—sometimes as early as 5 AM. There’s a quiet hum of the lab equipment that every embryologist knows. It’s a place of precision and concentration, where success can mean the difference between heartache and hope for a couple. Upon entering the lab, the embryologist takes a moment to check in (or inhale a coffee) and mentally prepare for the day ahead. They know that the morning can get hectic when things don’t run smoothly.
2. Calibrating the Equipment: Getting Everything to ‘Perfect’
Before handling any samples, an embryologist ensures that all of the lab equipment is properly calibrated. This is one of the most important steps in the IVF process, as even the smallest fluctuations in temperature, light, or humidity can affect the delicate embryos and their environment.
Some key pieces of equipment that need to be calibrated each morning include:
Incubators: Incubators are where embryos are placed to grow and develop in a controlled environment. Each incubator needs to be checked for temperature, humidity, and CO2 levels to ensure they’re optimal for embryo growth. A consistent environment is key for the survival of the embryos as they are cultured and prepared for transfer. Incubators can be tested with a Viasensor device.
Microscopes: The microscopes used to examine sperm, eggs, and embryos must be calibrated for clarity, focus, and illumination. These instruments are used for everything from sperm analysis to embryo grading, so precision is critical. Most microscopes now have tools attached to ensure certain moving parts are within calibrated ranges.
Pipettes and other handling tools: Precision instruments like pipettes, which are used to handle eggs, sperm, and embryos, must be checked for accuracy. A single drop of media can be crucial, and the right amount must be delivered at exactly the right moment. These tools are typically calibrated 1-2 times a year.
After checking and calibrating, the embryologist double-checks everything and ensures all instruments are sanitized, as sterility is essential in every part of the process.
3. Preparing Culture Media: The Secret Recipe for Success
When it comes to growing embryos, the environment is just as important as the initial ingredients. This step is not true for all labs and can vary. Some labs may prepare their culture media in the morning, but others prepare at the end of the day. Regardless, one of their main tasks is preparing the culture media. Culture media is a nutrient-rich solution that supports the embryos as they develop, mimicking the environment of the fallopian tubes or uterus.
There are several types of culture media used throughout the IVF process, each designed to meet the specific needs of embryos at different stages of development:
Fertilization Media: This media is used immediately after eggs are fertilized by sperm in the lab. It helps embryos to begin their initial stages of growth.
Cleavage Stage Media: At the cleavage stage, embryos are dividing rapidly. This media provides the nutrients embryos need to continue developing.
Blastocyst Stage Media: Once embryos reach the blastocyst stage, they are ready for transfer. The culture media is adapted to support embryos through this critical phase before implantation.
Each of these media solutions is carefully mixed, ensuring the pH is optimal, and the solution contains all the essential nutrients to nurture embryos. Technology has improved significantly and some companies will sell “single culture media” that supports all stages of development so there is manipulation between stages.
Once the media is ready, it’s placed in the incubators, where the embryos will be kept in the perfect conditions to grow and develop. Many don’t realize the importance of culture media and the preparation process. This is the environment nurturing the embryo so any micro changes or mistakes can severely affect the outcome. Just look into the situation with CooperSurgical media in 2024.
4. Checking Patient Files: Preparing for the Day’s Cases
Once the lab is set up and the media is ready, the embryologist reviews the patient files for the day’s cases. Every embryo, egg, and sperm sample is connected to a specific patient or couple, and all records must be accurate. At this point, the embryologist checks the following:
Sperm Analysis: Reviewing sperm quality and count to ensure that everything is optimal for fertilization.
Egg Retrieval Information: Looking over the timeline for the patient’s egg retrieval procedure to determine when eggs will be available for fertilization.
Fertilization Protocols: Each patient has their unique fertilization protocol, which may include traditional insemination or ICSI (Intracytoplasmic Sperm Injection). The embryologist makes sure they have the right equipment ready for each case.
Fertilization Checks: The embryologist will check the previous day's charts to ensure fertilization was successful.
Embryo Grading: The embryologist also reviews embryo progression and quality to anticipate how they may develop.
Plans can be changed and the last thing any embryologist wants is to perform the wrong procedure on an egg or embryo. Checking and preparing patient records is critical to the success of the rest of the day. Checks and balances or else disaster, just look back to this story from the California Center for Reproductive Health!
5. Collaborating with the Clinical Team
The first hour isn’t just about working alone in the lab; collaboration with the clinical team is an integral part of setting the IVF process in motion. The embryologist frequently communicates with doctors, nurses, and other team members to ensure the IVF process is seamless.
For example, if egg retrieval is scheduled for later in the day, the embryologist will touch base with the clinical team to ensure everything is lined up for optimal timing. The lab must be ready to handle the eggs and sperm immediately after the retrieval procedure.
The embryology team is not patient-facing so if any changes occurred, then it likely happened between the patient and clinical staff (doctor, nurse, medical assistant). This is why embryologists must have an open line to communicate with the clinical team. Communication of information is key to ensuring patients get the care and treatment they need. Is your IVF team communicating?
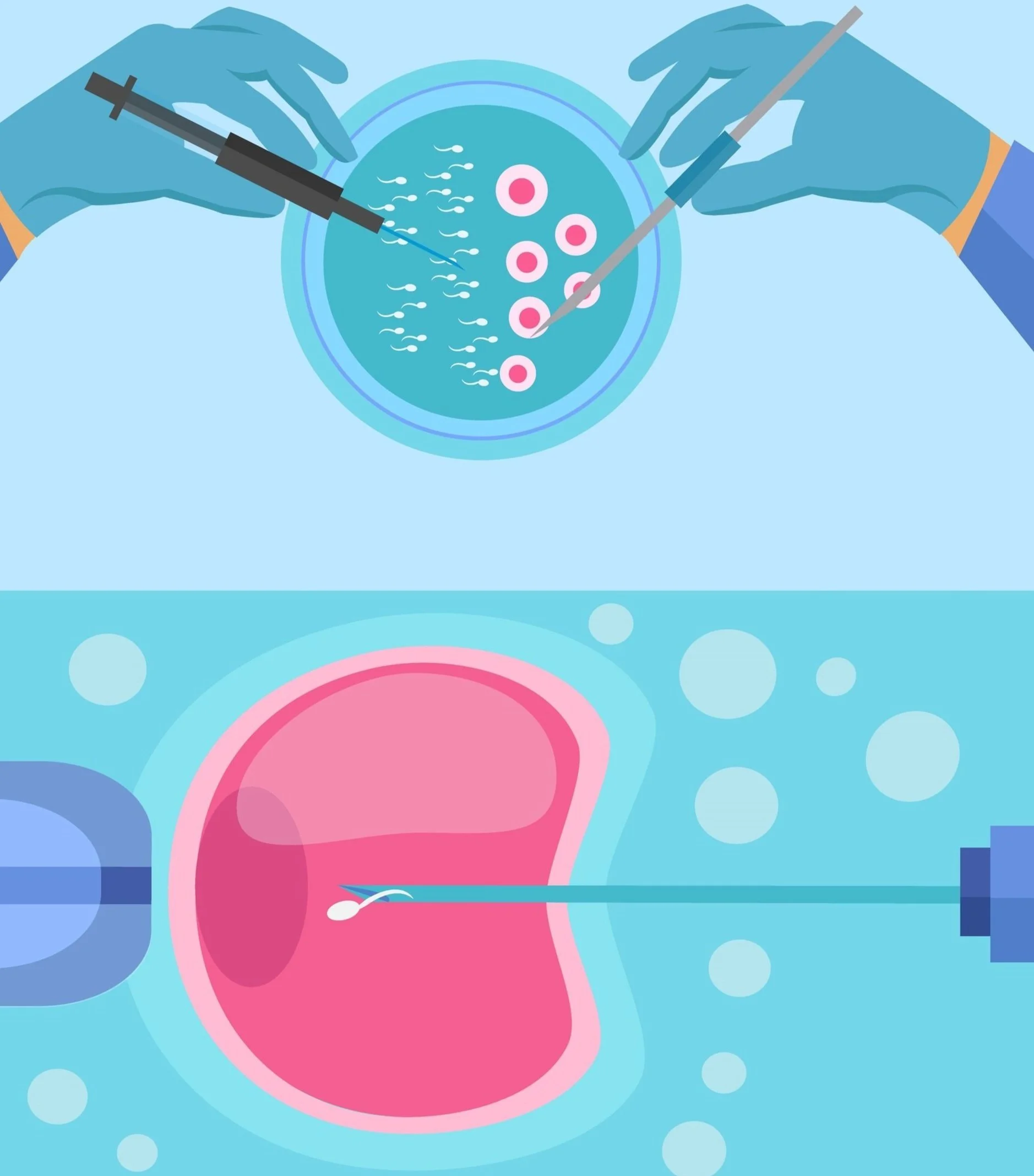
6. Getting Ready for Egg Retrievals: The Next Step
After all that, it is now time for the egg retrievals. The embryology team ensures all equipment is sterilized and culture media is prepped for the eggs and embryos. Embryologists work behind the scenes, setting up pipettes, microscopes, and incubators for a seamless retrieval process. Meanwhile, nurses and medical staff ensure the patient is comfortable and ready for the procedure. The goal is to create the perfect environment for successful egg collection, setting the stage for the next steps in the IVF process, which are critical for future embryo development.
Depending on your clinic, the embryologist may be in another room or in the same room as the patient.
Embryologist not in the room?
Likely that the patient is under anesthesia. The support nurse or medical assistant will pass the follicular fluid tubes through a window and the embryologist checks for eggs in the lab. This method could lead to the doctor missing eggs because they do not get direct and instantaneous notification when an egg is found. These patients are typically young with high follicular count so missing 1 or 2 may not be an issue.
Embryologist is in the room?
Likely the patient is awake. The support nurse or medical assistant will directly hand the follicular fluid tubes to the embryologist and they will check for eggs in the operating room. This method can be stressful because the embryologist must keep pace with the doctor so the patient has minimal pain and suffering. Speed and precision are key here. The bright side is doctors get instantaneous feedback and can prevent missing eggs from each follicle. These patients typically have lower follicular count so every egg counts.
7. Preparing for the Thaw: A Delicate Start to the Day’s Work
Can you believe this beautiful embryo is now a 10 year old?
Simultaneously as the egg retrievals, the embryology team must start the thawing of embryos and eggs. This step requires precise care, as the frozen embryos or eggs must be carefully thawed to ensure they survive the process and can be used for fertilization or implantation. Special thawing media is prepared, and the patient records are double-verified to ensure there are no mixups.
Timing is everything here. Too quick and the cells might be damaged; too slow and the cells may not thrive. Embryologists meticulously follow protocols, paying close attention to every detail, knowing that this crucial step sets the stage for the success of the IVF journey. It's a delicate balance of science and patience—getting everything just right for the embryos and eggs to flourish in the next stages of development.
This process happens behind the scenes, but it’s one of the first critical steps that ultimately leads to successful fertilization and embryo development, helping to create the best possible start for a family’s future.
8. The First Touches: A Smooth Transition to the Day’s Work
Just keep swimming
As the morning draws to a close, the embryology team must begin transitioning into the next phase of their day—working directly with the eggs, sperm, and embryos to move the IVF process forward. We will discuss this further another time!
Can you believe that everything you just read only amounts to 1-2 hours? An embryologist’s day is one of high focus and precision! One mistake can set back the entire team and worse it could have severe consequences to a patient’s cycle. Every step they take has a lasting impact on the fertility journey ahead.
Conclusion: A Quiet Foundation for Big Dreams
While patients may not always see the embryologist or understand the full extent of their work, the first hours in the IVF lab are vital. From calibrating equipment to preparing culture media, the embryologist lays the foundation for what could be a life-changing journey for a couple hoping to conceive. The precision, care, and attention to detail that goes into this quiet preparation are critical for ensuring that embryos grow and develop under optimal conditions.
So, while the first hours may be filled with meticulous prep work, it’s also the first step in a process that will unfold into something truly miraculous—bringing new life into the world, one carefully crafted embryo at a time.
Stay tuned for an afternoon in the life of an embryologist!
“Some people talk to plants; I talk to embryos. They don’t respond, but I swear they appreciate the encouragement.”