Behind Le Microscope: An Afternoon in the Life of an Embryologist
Following up from A Morning in the Life of an Embryologist, the pace inside the IVF lab shifts from preparation to action as the day transitions into the early afternoon. This is when the morning's groundwork bears fruit and the embryologist's role becomes even more intricate. Here’s a look at how afternoons unfold in the life of an embryologist, highlighting the critical tasks that make every minute count.
1. Egg and Embryo Assessments: Monitoring Progress
After completing morning procedures such as egg retrievals or thawing, embryologists turn their attention to assessing the progress of embryos. These evaluations determine the quality and stage of development for fertilized eggs. I briefly mentioned this in the morning role of an embryologist, but it can vary from lab to lab. Some labs are equipped with advanced time-lapse incubators, enabling embryologists to monitor and assess embryo development at any time with precision. In contrast, labs with standard incubators must conduct evaluations in the morning to ensure they capture critical developmental milestones, as these moments can otherwise be easily missed.
Fertilization Assessment: Embryologists evaluate fertilized eggs for proper development, assessing their quality by examining key indicators such as the presence of two pronuclei (2PN), symmetry, and the overall cellular structure.
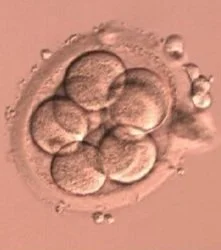
Cleavage-Stage Assessment: Embryologists check embryos for proper division, grading their quality based on symmetry, fragmentation, and cell number.
Blastocyst Formation Monitoring: Embryos are checked daily for progression into the blastocyst stage, which is crucial for implantation success.
Every observation made here is documented, as these findings guide the next steps in the IVF process, such as deciding which embryos to freeze or transfer. With advanced technology and AI, some companies are using these assessments to predict future outcomes in blastocyst formation and pregnancy rate.
2. Egg Denudation and Fertilization
After retrievals, eggs need to be stripped or denuded from their layer of cumulus cells (refer to the image). These cells support the egg during development by breaking down nutrients and delivering them directly to the egg. During denudation, the embryologist will use specific enzymes and tools to gently remove the cells of the egg. This step is crucial because it allows the embryologist to identify egg maturity. It is impossible to analyze eggs when they are covered by cumulus cells!
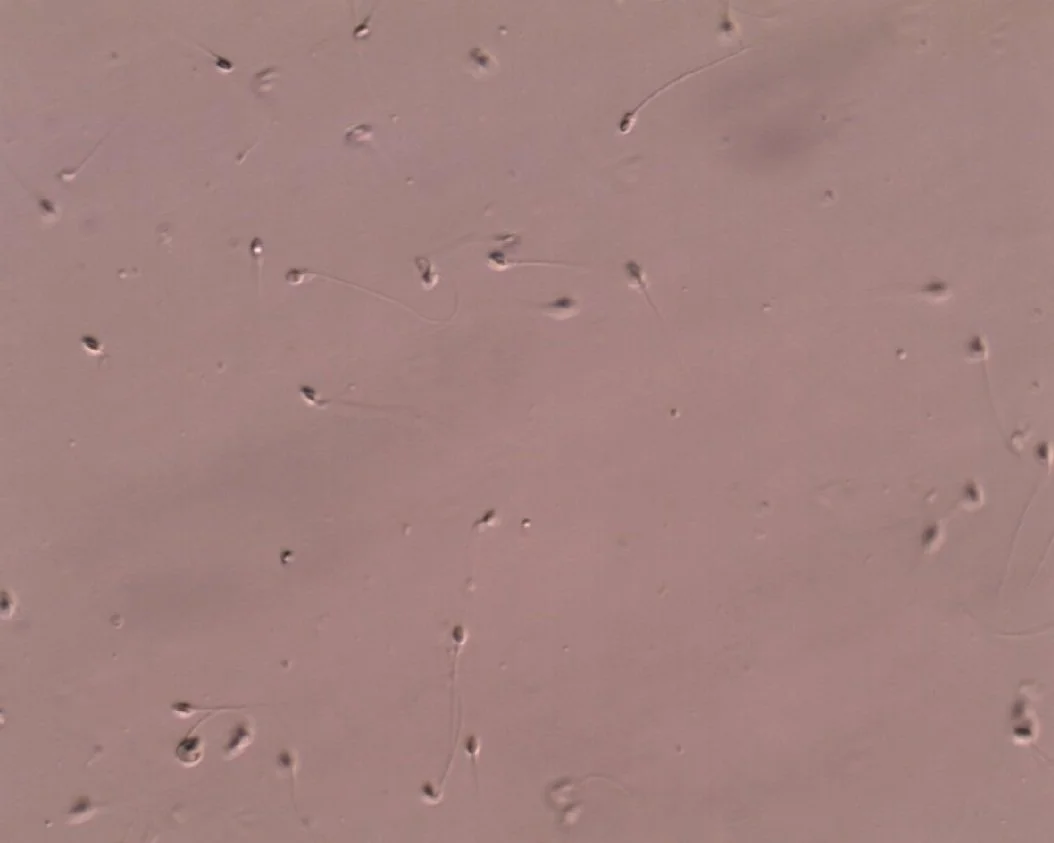
Once the mature eggs are identified, intracytoplasmic sperm injection (ICSI) begins. ICSI involves selecting a single healthy sperm and carefully injecting it directly into the egg’s cytoplasm using a fine glass needle. This precise technique bypasses many natural barriers to fertilization, ensuring the best chance of success, especially in cases of male factor infertility or low sperm count.
Another method of fertilization is called conventional IVF. In conventional IVF fertilization, mature eggs are placed in a culture dish alongside thousands of motile sperm, allowing fertilization to occur naturally. This method relies on the sperm’s ability to penetrate the egg independently, mimicking the natural process. It’s commonly used when there are no significant issues with sperm quality or quantity.
3. Sperm Preparation for Fertilization
As some eggs retrieved earlier in the day progress, sperm preparation for fertilization becomes a key task. This may involve:
Processing Fresh Samples: Preparing sperm samples that are typically given to the lab within 1-2 hours of retrieval
Processing Frozen Samples: Thawing and preparing frozen sperm samples for use.
Advanced Selection: Using techniques like motile sperm organelle morphology examination (MSOME), intracytoplasmic morphologically selected sperm injection (IMSI), or microfluidic sperm sorting (Zymot device) to ensure the best sperm quality.
How are we processing and preparing the sperm? Without getting too nerdy, the 3 most common lab techniques are
Simple Wash Process - Sperm are washed to remove seminal plasma and debris, yielding a concentrated pellet of sperm.
Swim Up Method - This involves letting the best sperm swim to the top of a tube by angling the tube to 45 degrees
Density Gradient - Sperm are separated by density using a gradient medium, isolating the healthiest and most viable sperm
4. Embryo Transfers
For many patients, embryo transfer is the most anticipated milestone in their IVF journey. In the afternoon, embryologists are often busy preparing for and assisting with this procedure.
Selecting the Embryo: The embryologist identifies the best-quality embryo for transfer based on their earlier assessments.
Loading the Catheter: Using sterile techniques, the embryo is carefully loaded into a catheter, ready for the transfer procedure.
Transfers are usually in the afternoon once all the egg retrievals are completed. The embryo is selected days in advance and thawed the morning of the scheduled transfer. It rests for 2 hours after thawing before being transferred back to the patient’s uterus. This is a complex procedure because sometimes it is hard to tell where the issue is if a patient did not get pregnant. Did the embryologist make a mistake? Did the doctor transfer into the wrong area? Is the patient’s body not ready to accept the embryo? Is embryo quality good enough?
All great questions that we can address another time.
5. Embryo Biopsy
Embryo biopsy is a delicate procedure performed during IVF to collect a few cells from an embryo, typically at the blastocyst stage, for genetic testing. This process helps identify chromosomally normal embryos (euploid) or detect specific genetic conditions, increasing the likelihood of a healthy pregnancy. The biopsy requires precision and expertise to avoid compromising the embryo’s viability, and the removed cells are analyzed while the embryo is frozen for later transfer.
The standard method for clinics now is trophectoderm blastocyst biopsy, but let us break down what we’ve done in the past
1. Polar Body Biopsy
When: Typically done at the oocyte stage before fertilization or after fertilization but before the first cleavage.
What: Involves removing one or both polar bodies from the oocyte or zygote.
Purpose: Provides information on the genetic material contributed by the egg, useful in detecting maternal chromosomal abnormalities.
2. Cleavage-Stage Biopsy
When: On Day 3, at the 6-8 cell stage of embryo development.
What: A single blastomere (cell) is removed from the embryo.
Purpose: Used to test for genetic or chromosomal conditions but is less common today due to concerns about embryo viability and mosaicism.
3. Blastocyst (Trophectoderm) Biopsy
When: On Day 5 or 6, at the blastocyst stage when the embryo has developed into a structure with distinct inner and outer cell masses.
What: Several trophectoderm cells (outer cells that form the placenta) are removed while leaving the inner cell mass (which will develop into the fetus) intact.
Purpose: The most common method today due to reduced impact on the embryo and the ability to test multiple cells for better accuracy.
4. Embryonic Cell-Free DNA Analysis (non-invasive)
When: During culture, without invasive biopsy.
What: Cell-free DNA is collected from the culture medium where the embryo is grown.
Purpose: A non-invasive method to test for genetic abnormalities, though not yet as widely validated or used as invasive biopsies.
5. Embryo and Egg Freezing (Cryopreservation)
Afternoons often involve cryopreservation of embryos that are ready to be frozen or have just been biopsied. Embryologists use specialized techniques to preserve the quality and viability of these embryos for future use.
Vitrification: This fast-freezing method minimizes the formation of ice crystals that could damage cells.
Documentation and Storage: Each embryo is carefully labeled and cataloged to ensure seamless tracking.
In the past, embryologists would slow-freeze, but this could take hours. Vitrification has truly been a groundbreaking advancement in the IVF field for embryologists and patients.
Embryos or eggs will go through a series of vitrification media, which prepares the egg to be frozen. After this process, they are loaded onto a thin straw and plunged into liquid nitrogen. Sounds dangerous, but is very safe! The straw will then be stored in a dewar tank until it’s ready to be transferred back to the patient.
7. Media Preparation
This was mentioned in the previous article, but each lab has different workflows and protocols. Some labs may prepare media in the early morning and others in the late afternoon.
Is one way better than the other? Both ways are good when done correctly!
8. Wrapping Up Cases and Preparing for Tomorrow
By late afternoon, embryologists begin organizing the day’s findings and preparing for the next day.
Final Checks: Embryos in culture are reviewed one last time, and notes are updated in the patient’s file.
Setting Up for Tomorrow: Supplies, media, and equipment are prepped for a seamless start in the morning.
Cleaning up: Stations are sterilized and wiped down. All dishes or tubes are discarded in the proper containers.
This routine ensures continuity of care, so nothing is left to chance.
Conclusion: We did it
An afternoon in the life of an embryologist is a mix of precision, adaptability, and collaboration. From monitoring embryos to supporting transfers, each task is imbued with the knowledge that their work is pivotal in creating life. These professionals embody the perfect blend of science and empathy, working tirelessly behind the scenes to turn hope into reality. Whether it's freezing embryos, coordinating with the team, or preparing for tomorrow, every moment counts in the IVF lab.
Each step in the lab is valuable and can be life changing. There is a long list of reasons why each step is critical to success, but we’ll save that for another time.
We hope you enjoyed this brief glimpse into the daily life of an embryologist. Let us know in the comments what you’d want us to discuss further!
“Turning cells into success stories—because even embryos need a pep talk and a push in the right Petri dish!”